|
<< Click to Display Table of Contents >> Payer Information and Rx Benefits Check |
  
|
|
<< Click to Display Table of Contents >> Payer Information and Rx Benefits Check |
  
|
This chapter discusses the Payer Information and Rx Benefit Check options.
Real Time Formulary is the SureScripts process wherein real-time Request and Response messages (271 information) are received and the Payer Information will populate to the bottom of the Prescription Edit screen. This provides data that informs the prescriber of the medication's formulary status, payer-provided alternatives, coverage factors, and copay details.
There are two message types associated with the Real Time Formulary and Real Time Prescription Benefits functionality:
•The Benefit Request message is used to request representative formulary information or patient-specific estimated cost and benefit information. The message content and endpoint will dictate whether representative formulary (RFS) or patient specific (RTPB) estimated cost and benefit information is returned in the Benefit Response.
•The Benefit Response message returns representative formulary information or patient-specific estimated cost and benefit information, or the response may return business errors (e.g., Patient Not Found, Unknown Formulary ID, etc.). The information contained in the Benefit Response is dictated by the Benefit Request workflow and content.
Select Web Client > Charts > Select Patient > Prescription Entry > New Rx > Select Medication > Selected Payer options will populate
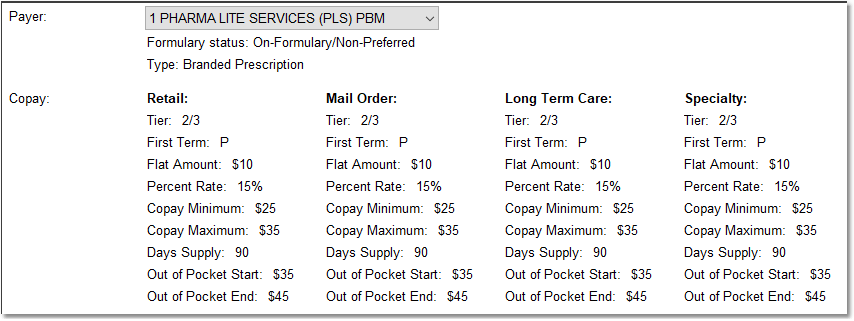
Prescription Edit screen - Payer section
Select Web Client > Charts > Select Patient > Prescription Entry > New Rx > Select Medication > Prescription Edit
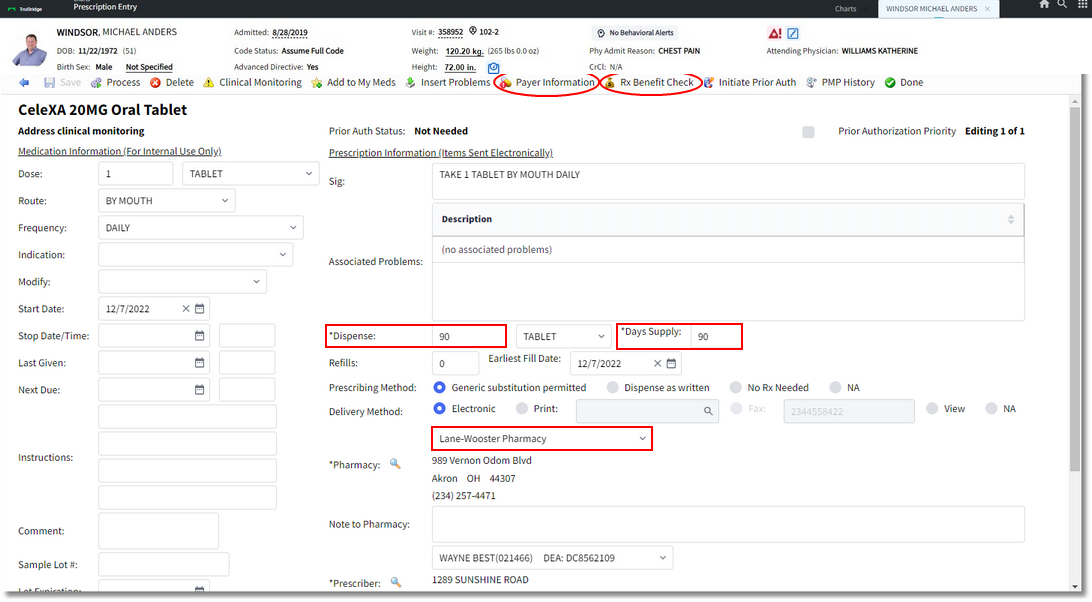

Prescription Edit Screen
▪Payer: After the drug has been selected, the system automatically retrieves the patient’s payer information, which is provided by SureScripts. The Payer field will then display any formulary or coverage data. The data can include copay information or preferred alternative drugs if the selected medication is not on the formulary for the payer.
oIf alternative medications are available based on the PBM, this will enable the Coverage and Formulary button on the action bar.
oIf alternative medications are not available based on the PBM, the Coverage and Formulary button will be disabled.
Coverage and Formulary/Payer
•Once the medication has been selected, a coverage and formulary screen will display to notify the user if the current medication is on formulary with the patient's insurance.
NOTE: An eligibility request is automatically generated and sent when the visit is created. If no visit is created, the system will retrieve the information at the time of prescription entry. It is a standard 270/271 format. Coverage status is viewable during prescription entry.
Select Web Client > Charts > Select Patient > Select Account > Prescription Entry > New Prescription > select Medication > Payer
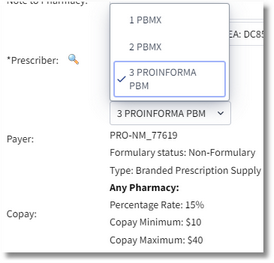
Payer
To view the Coverage Restrictions/Coverage and Formulary Information, select the Payer Information (if enabled) option. The screen will return results for the selected payer. Use the back arrow to return to the previous screen.
Select Web Client > Charts > Select Patient > Select Account > Prescription Entry > New Prescription > select Medication > Payer Information
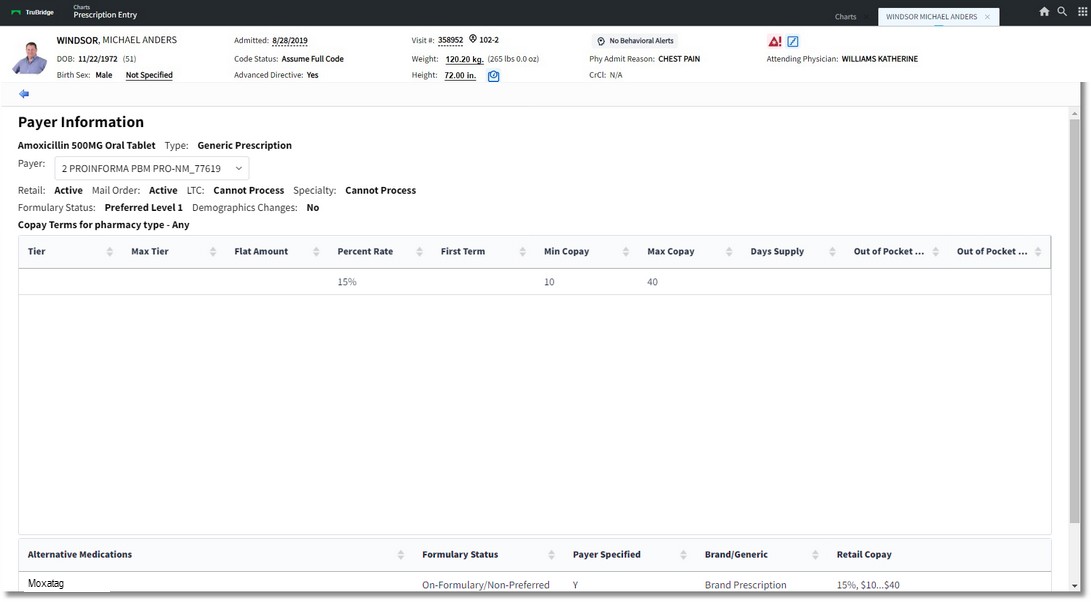
Coverage and Formulary Information
•If the medication is on formulary, the formulary status will display the Payer (formulary alternatives), formulary status and Co-pay Terms for pharmacy type.
▪If the patient is not in the Surescrips database, e.g. a newborn without coverage information or someone who has never had prior insurance coverage, the user will see a message at the bottom of the Formulary screen display. The message will read, "Rejection received from eligibility request. The formulary information may not be accurate. Rejection code: 75 Subscriber/Insured Not Found Resubmission Not Allowed." This will not prevent the user from entering the medication.
•If it is not on formulary, a list of Preferred Alternative Drugs will populate at the bottom of the screen. Once the medication has been selected, the user will select Continue. If the Restrict Payer Disclosure option is selected on the Guarantor/Ins tab in the Registration and ADT screens, the Prescription Entry screen will display. The only options available will be Print and View in Prescription Writer. Please refer to the Person Profile and Registration User Guide for more information on the Restrict Payer Disclosure option.
▪If a medication is selected from the Preferred Alternatives list, the system will present formulary information on the medication. Even if the medication is on formulary, there may be additional coverage rules and/or information.
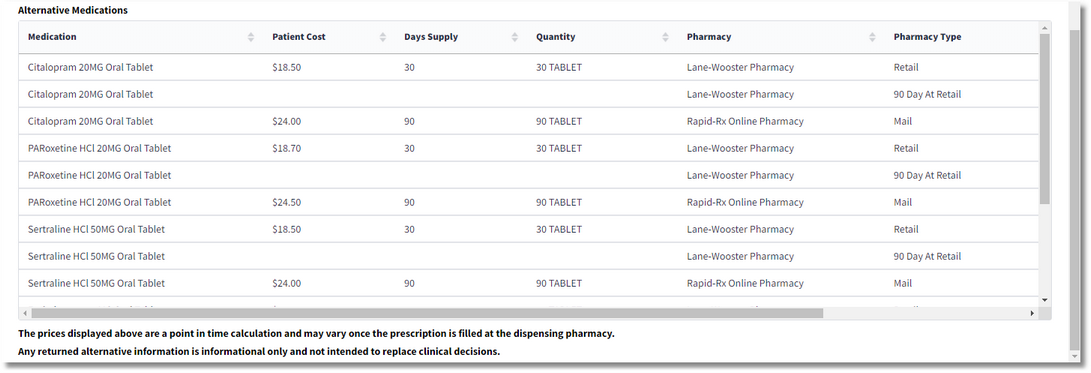
Real Time Prescription Benefits is a real-time Request and Response message between the provider vendor and PBM. The RTPB message is designed to give provider a real-time estimated cost for the specific patient, allowing the prescriber to make prescription decisions at the point of care. Once the Medication with a valid NDC number, Days Supply, Dispense Quantity, Quantity Unit of Measure, and Pharmacy have been selected, the provider vendor automatically sends a Benefit Request for patient specific estimated cost and benefit data. SureScripts receives the Benefit Request message and requests patient benefit information from the PBM/Payer. The PBM/Payer will then process the request and format a Benefit Response message with patient specific cost and benefit information and sends to SureScripts, which will forward the Benefit Response synchronously to the provider vendor. The provider may then select the Benefit Checking option and select the Requested Medication or Alternative Medication. The message information will include point-in-time estimated cost, alternative medication options, pharmacy type options, and formulary information. The data is referenced prior to the NewRx to inform the prescriber and patient of the specific estimated out-of-pocket cost for the selected therapy. If an Alternative is selected, then a new prescription will be created for that item. Alternative medications shall be displayed in the order they're in from the response.
If the prescriber selects an alternative medication that references a sunset QuantityUnitOfMeasure code, the prescriber should send a valid QuantityUnitOfMeasure. The BenefitResponse AlternativeMedications section will need to be compared to what is current.
•If the alternative medication is selected, the current logic of auto-populating the Dispense Unit should still be present.
•If no match is found, the Dispense Unit should be blank. The Dispense Quantity and Dispense Unit fields will be red to indicate that they are required.
SureScripts has updated their RTF benefit request standards to only allow up to 250 Alternative Medications to be sent in the request.
The bottom the the screen will display verbiage regarding how the user shall be made aware that the above pricing data is a point in time calculation based and may vary once the prescription is filled at the dispensing pharmacy. Any returned alternative information is informational only and not intended to replace clinical decisions.
Rx Benefit Check: Once a medication or therapeutic alternative has been selected, the provider sends the Benefit Request for representative formulary data. SureScripts then processes the benefit Request message, gathers the applicable representative formulary data (information listed above) and returns a Benefit Response to the provider vendor The prescriber may then select the Alternative Meds/Restrictions option from the action bar. This will only be available to select if any Coverage and Formulary alternatives or restrictions exist for the selected payer. The requests may be used for a period of up to 24 hours and will have to be resent if that time frame is exceeded.
Select Web Client > Charts > Select Patient > Prescription Entry > New Rx > Select Medication > Prescription Edit > Rx Benefit Check
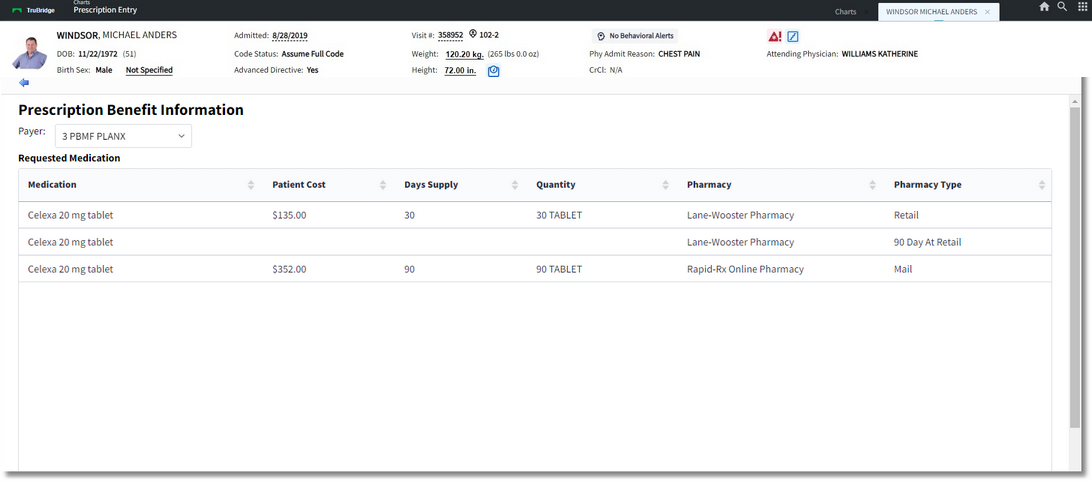
Prescription Benefit Information
Message IDs
•For an RTF Benefit Request, the RelatesToMessageID tag should be in the ICN from the eligibility response.
•For an RTPB Benefit Request, the RelatesToMessageID tag should be the ICN from the eligibility response.
•For NewRX message, the RelatesToMessageID tag should be the MessageID from the RTF Benefit Response if an RTPB Benefit Request is never sent and, subsequently, an RTPB Benefit Response is never received. If an RTPB Benefit Response is received, then the MessageID from the RTPB Benefit Response should be used for the RelatesToMessageID tag.